When a comet assay, an increasingly popular in vivo genotoxicity test, shows a positive test result, interpretation of that response requires ruling out any confounding tissue site toxicity. Since the comet assay typically uses only 2 or 3 daily doses of test agent, precursor tissue changes indicative of toxicity may be easily overlooked. Using case examples for two flavoring agents, perillaldehyde and 4,5 -epoxydec-2(trans)-enal, we highlight the role of pathology peer review in verifying precursor tissue changes indicative of tissue site toxicity, thereby increasing confidence in final interpretation of comet assay results. Given global deliberation regarding safety assessment of compounds entering the marketplace, we recommend consideration of pathology peer review for equivocal and positive comet assays so that interpretations are universally consistent.
Introduction
Safety assessment of flavoring agents includes successful completion of a battery of in vitro and in vivo genotoxicity assays. When in vitro assays such as the bacterial reverse mutation assay, the in vitro micronucleus assay, or the hypoxanthine phosphoribosyltransferase (HPRT) mutation assay in L5178Y lymphoma cells show positive or equivocal results, regulatory authorities may request an in vivo genotoxicity assay such as a rodent micronucleus and/or comet assay. The comet assay, also known as the single cell gel electrophoresis assay, is a sensitive technique for detection of DNA strand breaks in eukaryotic cells. It may be conducted in mice or rats on most any tissue type and combined with a micronucleus assay and/or integrated into a repeated dose toxicity study. The liver is typically the preferred tissue for evaluation in the comet assay because it is the most active organ in the metabolism of substances and is frequently a target organ for carcinogenicity; other tissues are selected for evaluation based on any knowledge of a potential mechanism or as site-of-contact tissues most relevant to exposure. As discussed below, histopathology on tissues evaluated in the comet assay represents an important component in interpretation of test results.
Two flavoring agents have recently been tested in genotoxicity assays, including comet assays that heavily relied on histopathology to provide contextual relevance for interpretation of the results. Perillaldehyde (also known as p-mentha-1,8-dien-7-al) is a natural compound in the herb perilla and in the peel of citrus fruits. The isolated chemical from perilla, as well as a chemically synthesized version, is used as a flavoring agent to add a fatty-spicy, oily-herbaceous aroma to a variety of foods and beverages. The second flavoring agent, 4,5-epoxydec-2(trans)-enal, is also a naturally occurring flavoring substance found in various foods/beverages such as orange juice, tea, and dairy products. It can form as a degradation product of fats in many foodstuffs. Because it exists only at a very low level in natural sources, synthesized chemical is used as a flavoring in foods and beverages.
Using perillaldehyde and 4,5-epoxydec-2(trans)-enal as case studies, the purpose of this report is to show the relevance and importance of pathology peer review and to emphasize the need for global harmonization in using pathology peer review as an aid in the evaluation and interpretation of positive comet assay results.
Comet assay background
The comet assay is a technique to detect DNA strand breaks in eukaryotic cells. It has gained popularity in genotoxicity testing, especially following acceptance of an Organization for Economic Co-operation and Development (OECD) test guideline for the comet assay in rodents1. It is considered a useful follow up test in situations where in vitro genotoxicity assays show positive or equivocal results2. It is also often used to meet the second in vivo assay requirement of Option 2 of the standard test battery outlined in the International Conference on Harmonisation (ICH) S2(R1) guidance for genotoxicity testing of pharmaceuticals (http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Safety/S2_R1/Step4/S2R1_Step4). Tissue cells to be investigated are embedded in agarose on a microscope slide and their cell membranes lysed with detergent and high salt concentration to form nucleoids containing supercoiled loops of DNA attached to the nuclear matrix. During electrophoresis at high pH, undamaged DNA remains in the nucleoid while negatively charged fragmented DNA migrates out of the nuclear matrix and moves toward the anode creating a trail that, when examined by fluorescence, resembles a comet tail. The intensity and length of the comet tail relative to the comet head that has undamaged supercoiled DNA is an indication of the extent of DNA strand breaks and is assessed microscopically either manually or using image analysis software.
In applying the comet assay as part of a genotoxicity battery of tests, rats or mice are dosed with a test agent of interest and cells are collected for the comet assay shortly after a second or third daily dose. The dosing and harvest regimen is designed to provide sufficient time for metabolism of the test substance while also allowing for detection of strand breaks prior to DNA repair. Multiple dose levels of the test agent plus vehicle and positive (e.g., ethyl methanesulfonate) controls constitute a typical test that often includes clinical chemistry and histopathology to check for any toxicity that could confound results. The comet assay may be combined with an in vivo erythrocyte micronucleus test and/or incorporated into a repeated dose toxicity test to conserve animal use. Details regarding comet assay testing parameters are readily available1,3-5 and will not be covered here.
Interpretation of comet assay results is conventionally based on four parameters:
- whether or not at least one test dose is statistically significant versus the concurrent control
- whether or not there is a statistically significant positive trend analysis reflecting a dose response
- where data points fall with respect to laboratory historical control data
- demonstration of exposure of the examined tissue(s) to the test agent.
Assessment of exposure/toxicity may be based on clinical signs (e.g., ataxia, piloerection, abnormal or prone posture, loss of body weight, reduced activity), toxicokinetics, clinical chemistry, urinalysis, and histopathology. DNA damage due to chemical-related cytotoxicity or to excessive mechanical disruption during cell isolation can confound interpretation of comet assay results. Therefore, for a given dose to be considered positive, there should be no evidence of excessive toxicity to the examined tissue at that dose. Although the OECD test guideline mandates that the frequency of “hedgehog” cells [a morphology indicative of highly damaged cells which can be associated with severe cytotoxicity, necrosis or apoptosis4-6; also known as “clouds” and “ghosts”] be determined, there is no consensus as to just how these data should be factored into interpretation of results. The international validation of the in vivo comet assay for the detection of genotoxic carcinogens, coordinated by the Japanese Center for the Validation of Alternative Methods (JaCVAM), led to the conclusion that histopathology remains the “gold standard” for assessing tissue cytotoxicity, and that changes in % tail DNA require careful interpretation when measured in conjunction with severe histopathological changes3.
Pathology peer review background
Since pathology diagnosis is qualitative and subjective, a pathology peer review increases confidence in the pathology assessment by assuring the quality of the study animal observations and the pathology diagnoses and their interpretation. The pathology peer review process involves examination of the study pathologist’s (SP) diagnoses and his/her interpretation of pathology study findings by an expert in diagnostic histopathology. The pathology peer review may take place on site at the performing laboratory or remotely and the timing of the review may occur before or after finalization of the SP’s diagnoses and interpretation. In either case the pathology peer review should be planned, managed, and documented.
Although not mandated by Good Laboratory Practice (GLP) guidelines, pathology peer review is endorsed by regulatory authorities as a means for verifying and improving the quality of the pathology data and increasing confidence in the accuracy of the qualitative and subjective nature of pathology diagnoses and interpretation. Recent publications cover procedural considerations and details involved in pathology peer review7,8. There are two situations where regulatory authorities require a pathology peer review. The U.S. Environmental Protection Agency (EPA) requires pathology peer review if a compound is being re-registered and the European Medicines Agency (EMA) requires a pathology peer review for carcinogenicity studies of medicinal products8.
Case examples
Case examples highlighting the importance of pathology peer review are provided for two flavoring agents: perillaldehyde and 4,5-epoxydec-2(trans)-enal. The European Food Safety Authority (EFSA) evaluation of these two substances was conducted without the benefit of a pathology peer review and concluded potential genotoxicity for both flavoring agents based (in part) on comet assay results. Subsequently, a pathology peer review was requested by Japan Flavor and Fragrance Materials Association (JFFMA) which was conducted by an expert in diagnostic histopathology; evidence of toxicity was identified at comet assay doses considered positive by EFSA.
Perillaldehyde
Perillaldehyde is a natural organic compound present in the essential oils of fruits, berries and herbs9. It is used in perfumery and has a mint-like cinnamon odor. As a flavoring agent it adds a fruity and spicy flavor to a variety of beverages, baked goods, frozen dairy products, gelatins and puddings, and in soft candy10.
Perillaldehyde has recently been tested in genotoxicity assays including the comet assay. It is ‘generally recognized as safe’ (GRAS) by the Expert Panel of the U.S. Flavor and Extract Manufacturers Association (FEMA)11. It is also judged safe by the Food and Agriculture Organization (FAO)/World Health Organization (WHO) Joint Expert Committee on Food Additives (JECFA)12 and unlikely to harm human health according to the Japanese Food and Sanitation Act (http://www.mhlw.go.jp/english/topics/foodsafety/foodadditives/index.hjtml).
Perillaldehyde genotoxicity testing results were recently reviewed by a FEMA expert panel that concluded that perillaldehyde has no apparent in vivo genotoxic potential13.
Perillaldehyde, a monocyclic terpenoid with an a,b-unsaturated functional aldehyde group, is rapidly metabolized with excretion unchanged or as conjugated carboxylic acid12. Based on structural alerts for possible genotoxicity of a,b-unsaturated aldehydes and ketones, perillaldehyde was selected for additional genotoxicity testing as representative of subgroup 2.2 of EFSA’s Flavouring Group Evaluation 19 (FGE.19)14,15. The comet assay was among the studies carried out by interested industries. Study details for the comet assay as well as a micronucleus assay in rats, a bacterial reverse mutation assay, an in vitro micronucleus assay in human lymphocytes, and an in vitro HPRT mutation assay in L5178Y mouse lymphoma cells have been published10. Perillaldehyde induced mutations in Salmonella typhimurium strain TA98 without metabolic activation. There was no evidence of genotoxicity in the in vitro micronucleus assay, the HPRT assay, and the micronucleus assay in male Wistar rats.
In combination with the in vivo micronucleus assay16, a comet study was conducted in male Wistar rats17 in accordance with recommendations from EFSA and expert working groups2,4,5, and generally consistent with the subsequently published OECD guideline 4891. Following a dose range-finding study with no gender differences, male rats were administered perillaldehyde by oral gavage at doses of 175, 350 and 700 [the estimated maximum tolerated dose (MTD)] mg/kg/day for three successive days with a corn oil vehicle control and an aqueous ethyl methanesulfonate (150 mg/kg/day) positive control. Animals (6 rats per treatment group) were sacrificed 3 hours following the final dose. Blood was collected for clinical chemistry and liver and duodenum tissues were prepared for the comet assay and fixed for histopathology. Comet data were captured using an automated imaging system (Comet Assay IV; Perceptive Instruments, Suffolk, UK).
Results of the comet assay are presented in Table 1. There was no indication of DNA damage in the duodenum of perillaldehyde-treated rats. Liver tissue from rats exposed to the highest dose (700 mg/kg/day) was associated with a small, but statistically significant, increase in % comet tail intensity, and there was a statistically significant linear trend. While the % tail intensities for all 6 rats in the 700 mg/kg/day group were within the laboratory’s historical vehicle control 95th percentile range, the % tail intensity for 5 of these rats exceeded intensity levels in the concurrent controls. A statistically significant increase in DNA damage was measured in the duodenum and liver for the positive control group.
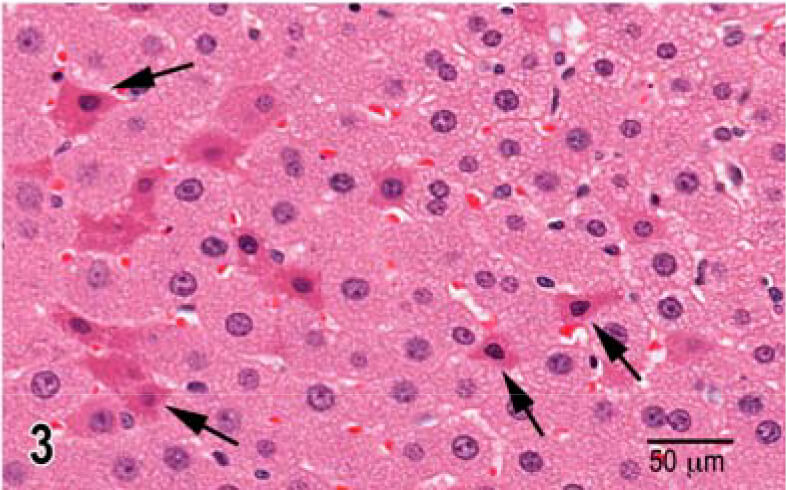
Post dosing clinical observations on day 3 following administration of 700 mg/kg/day perillaldehyde included a reduced level of activity in 5 of 6 rats and ataxia and piloerection in 1 of 6 rats. No macroscopic changes associated with exposure to perillaldehyde were present. The initial histopathologic findings in liver tissue evaluated by the SP was limited to hepatocyte vacuolation in rats receiving 700 mg/kg/day. In the subsequent pathology peer review of the liver slides, hepatocyte enlargement was present in all 6 rats administered 700 mg/kg/day. In contrast to control rats (Fig. 1), there was periportal to mid-lobular microvesicular cytoplasmic vacuoles consistent with fat, and the hepatocyte enlargement caused compression of sinusoidal channels (Fig. 2). Centrilobular hepatocyte degeneration characterized by loss of cytoplasmic and nuclear detail was occasionally present in these rats. Individual and small aggregates of hepatocytes with condensed nuclear chromatin and hypereosinophilic shrunken cytoplasm were present to varying degree only in the 700 mg/kg/day dose group (Fig. 3). Three of the 6 rats in this highest dose group had high, but not statistically significant, serum alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels, indicative of hepatic toxicity. Statistically significant elevation of serum urea and decreased cholesterol, glucose, and electrolytes (sodium, chloride, potassium) supportive of general toxicity were also present in the high dose group. In light of evidence of hepatotoxicity in the 700 mg/kg/day perillaldehyde rats, and the % tail intensity results falling within laboratory historical data, the comet results in this group are considered secondary to toxicity and not a direct effect of perillaldehyde.
4,5–Epoxydec-2(trans)-enal
4,5-Epoxydec-2(trans)-enal is used as a fragrance and flavoring agent in a variety of foods including canned orange juice, breads, various cooking oils, buttermilk, boiled cod, and popcorn18. It is used to enhance the flavor and/or odor of a variety of foods and has a citrus odor and fruity mandarin orange flavor. It can be formed during baking with fats containing linoleic acid.
4,5-Epoxydec-2(trans)-enal was evaluated for genotoxicity as a representative of subgroup 1.1.1(b) of FGE 19 in FGE 226 aliphatic aldehydes with a,b-unsaturation conjugated with an epoxide moiety that is considered a structural alert. It was previously considered to have no safety concerns at current levels of intake by JECFA19,20. As referenced by EFSA, a bacterial reverse mutation assay was negative and in vitro micronucleus assays in human peripheral lymphocytes gave equivocal, positive, and negative results in successive assays18. An in vivo micronucleus assay conducted in Han Wistar rats, while negative for genotoxicity, was considered unreliable since there was no evidence of bone marrow exposure18. A rat comet assay was recommended by EFSA.
For the comet assay, an MTD of 350 mg/kg/day was determined based on a dose range-finding study in Han Wistar rats with no gender difference in response. Consequently, a comet assay was designed with 6 male rats per group. Groups included a 0.5% aqueous methylcellulose vehicle control, an ethyl methanesulfonate positive control group (150 mg/kg), and treatment groups administered 75, 150 and 300 mg/kg/day of 4,5-epoxydec-2(trans)-enal by oral gavage. Rats were sacrificed 3 hours following the second day of dosing, blood was collected for clinical chemistry, and liver and duodenum tissues were prepared for the comet assay and fixed for histopathology. Comet data were captured using an automated imaging system (Comet Assay IV; Perceptive Instruments). Study design details are provided in a company report21.
Comet assay results for the duodenum were negative (data not shown). Results of the comet assay for liver are presented in Table 2. A statistically increased mean % tail intensity was observed in groups receiving 75 and 300, but not 150, mg/kg/day of 4,5-epoxydec-2(trans)-enal with a statistically positive trend and with all individual values falling well within the laboratory’s historical control 95% reference range.
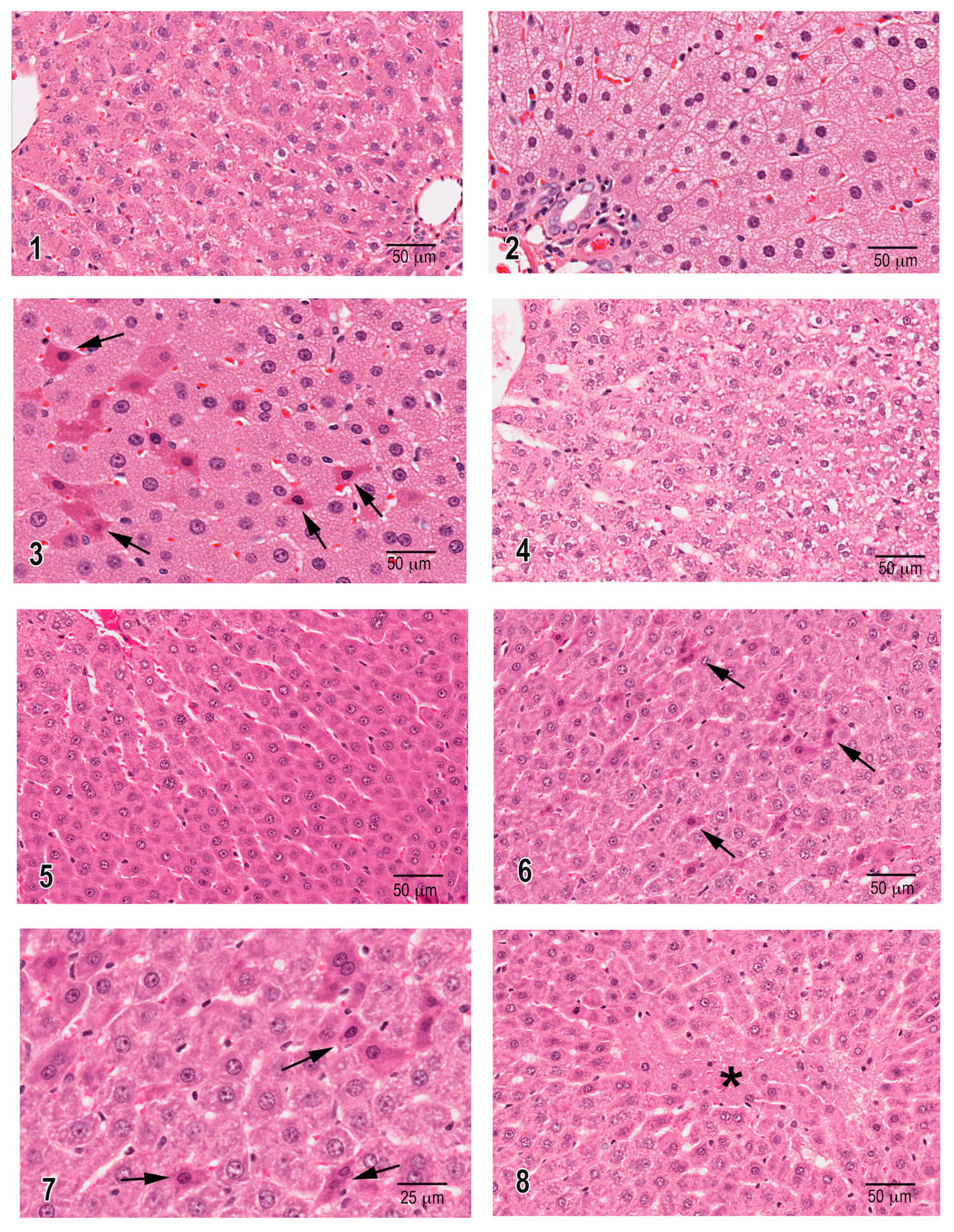
There was a small dose-related reduction in body weight gain resulting in body weight loss at the 300 mg/kg/day dose group. There was a dose-related increase in serum albumin, total protein, the albumin/globulin ratio and serum phosphorus and a dose-related decreased mean serum calcium. One rat given 300 mg/kg/day of 4,5-epoxydec -2(trans)-enal had a marked increase in serum urea and creatinine and the highest serum AST and ALT, with the ALT 3 times higher than the control group mean ALT. In addition, small increases in serum urea were recorded in several rats administered 300 and 150 mg/kg/day of 4,5-epoxydec-2(trans)-enal. Since the rats were not fasted before termination, control livers contained irregular clear cytoplasmic spaces consistent with glycogen (Fig. 4). The SP reported a minimal to slight decreased hepatocyte glycogen in all 4,5-epoxydec–2(trans)-enal treated groups with a dose response (Fig. 5). During the pathology peer review, liver changes were noted in the rats administered 300 mg/kg/day where there was a prominent increase in hypereosinophilic hepatocytes in multiple areas in both liver sections provided for each of the 6 rats (Fig. 6). The hypereosinophilic hepatocytes had angular cytoplasmic membranes, condensed hyperchromatic nuclei, shrunken and mis-shaped nuclei, and often had evidence of condensed ribosomal cytoplasmic deposits (Fig. 7). These liver changes represent features of progression from early degeneration to cell death. Clear evidence of centrilobular hepatocyte necrosis was present in one of the six high dose rats (Fig. 8). It is noted that one rat in each of the lower doses had rare occurrence of hypereosinophilic hepatocyte cytoplasm, likely representing biological variability in susceptibility. Taken together, the clinical signs, clinical chemistry changes and morphological evidence of hepatocellular degeneration and necrosis reflect hepatotoxicity at the 300 mg/kg/day dose level.
Discussion
Current genotoxicity test guidelines mandate that, unless precluded by use of the limit dose, exposure of an examined tissue to the test agent be demonstrated. In lieu of direct measurement of a test agent or its metabolite in tissues by bioanalytical methods, which can be costly and burdensome, this criterion for a valid test may sometimes be achieved by demonstrating adverse clinical signs indicative of reaching the MTD and/or detection of evidence of toxicity in relevant tissues. Since toxicity can lead to confounding results in the comet assay, accurate assessment of tissue cytotoxicity is imperative. During the JaCVAM validation trial of the in vivo comet assay, a standardized approach for presenting and interpreting histopathological findings was deemed necessary3. It was concluded that necrosis and/or findings indicative of degenerative changes would be the main indicators of cellular toxicity, whereas apoptosis could indicate both cellular toxicity and DNA damage. Furthermore, it was determined that grade and incidence of histopathological changes should be considered in the interpretation of cytotoxicity in relation to positive comet results.
The conduct of the comet assay typically involves a relatively short 2- or 3-day exposure to a test agent without sufficient time for classical hepatotoxicity to be clearly manifested. Furthermore, given that the main endpoint in a comet assay is assessment of the comet tails, the follow-up histopathology is likely to be a somewhat casual examination, on the lookout for obvious and prominent evidence of hepatic lesions such as coagulation necrosis or evidence of inflammatory cellular infiltrates secondary to necrosis. But even with very careful and detailed histopathological examination, the diagnoses and interpretation remain subjective, influenced by the experience of the study pathologist. Consequently, a pathology peer review is always beneficial to confirm initial histopathologic findings and their interpretation and increase confidence in study pathology findings. For this very reason, regulatory authorities favor receiving evidence of a pathology peer review and, in questionable or critical situations, regulatory agencies may strongly suggest or even request a pathology peer review. For the two cases presented in this report, detailed examination of the liver sections during the pathology peer review identified morphological evidence of early hepatotoxicity that should be considered in evaluation of positive comet assays.
In the two examples highlighted in this report, EFSA evaluated the results of the comet assays based on the available information at the time of their final determination. EFSA did not have the benefit of the pathology peer review findings of histopathological hepatic changes when evaluating perillaldehyde and 4,5-epoxydec-2(trans)-enal comet assay data. The results of genotoxicity testing of perillaldehyde, including the pathology peer review findings, were recently reviewed by a FEMA expert panel that concluded there is no apparent in vivo genotoxic potential13. As indicated earlier, 4,5-epoxydec-2(trans)-enal was previously considered to have no safety concerns at current use levels19,20.
Contemporary growth of international commerce has fostered a consumer interest in ethnic food products and allowed for global availability of ethnic and country-specific foods and beverages. Many of these foods and beverages contain flavoring substances that impart, enhance and/or modify flavor and/or aroma. In a 2015 publication, it was estimated that about 3250 flavoring substances are in use in Japan, 2500 in Europe, and 2,300 in the USA22. Genotoxicity assays are a component of the safety assessment of food additives such as flavoring agents and are conducted in various countries. The Konishi et al. publication22 indicates the need and importance of international harmonization of these as well as other safety assessments. Given global considerations regarding safety assessment of compounds entering the marketplace, it is important to harmonize standards for conduct of pathology peer review such that the process is transparent, and interpretations are consistent.
The two flavoring agents highlighted in this report are each considered representative of a class of flavoring substances. Consequently, the outcome of their hazard assessment has implications for the remaining members of their respective chemical classes. Perillaldehyde and 4.5-epoxydec-2(trans)-enal were evaluated in Europe by EFSA and judged to have genotoxic potential15,18. At the same time, these two flavoring agents are permitted in food products in the USA and Japan where they are judged to be safe at current usage levels by regulatory authorities and scientific bodies such as JECFA, FEMA Expert Panel, U.S. Food and Drug Administration (FDA) and Japanese Ministry of Health, Labour and Welfare (MHLW). The EFSA judgment that these two flavoring agents have genotoxic potential, based on statistically positive comet assays, and determined without the benefit of a pathology peer review that identified hepatotoxicity, stands in contrast to the opinions of these other scientific bodies. Whether having the findings of the pathology peer review histopathology and interpretation in advance would have influenced the EFSA judgment regarding the genotoxicity hazard of perillaldehyde and 4,5–epoxydec-2(trans)-enal remains an open question.
Clearly, the field would benefit from a greater mechanistic understanding of the specific histopathological findings that correlate with confounding effects on the comet assay. Moreover, improved harmonization of testing and data interpretation standards for safety assessment as well as submission of peer-reviewed subjective study results will lead to greater confidence in data and better regulatory decisions in hazard identification. Towards that end, we believe there is an important role for pathology peer review in safety assessment of food additives, including flavorings, as well as other test agents that have a positive or equivocal comet assay response.
Acknowledgements
We are grateful for editing assistance provided by Fumiko Sekiya of the Japan Flavor and Fragrance Materials Association.
References
- OECD Guideline for the Testing of Chemicals. 489 In Vivo Mammalian Alkaline Comet Assay. 2016.
- Minimum criteria for the acceptance of in vivo alkaline comet assay reports. EFSA J. 10: 2977. 2012.
- Uno Y, Kojima H, Omori T, Corvi R, Honma M, Schechtman LM, Tice RR, Beevers C, De Boeck M, Burlinson B, Hobbs CA, Kitamoto S, Kraynak AR, McNamee J, Nakagawa Y, Pant K, Plappert-Helbig U, Priestley C, Takasawa H, Wada K, Wirnitzer U, Asano N, Escobar PA, Lovell D, Morita T, Nakajima M, Ohno Y, and Hayashi M. JaCVAM-organized international validation study of the in vivo rodent alkaline comet assay for detection of genotoxic carcinogens: II. Summary of definitive validation study results. Mutat Res Genet Toxicol Environ Mutagen. 786-788: 45-76. 2015.
- Tice RR, Agurell E, Anderson D, Burlinson B, Hartmann A, Kobayashi H, Miyamae Y, Rojas E, Ryu JC, and Sasaki YF. Single cell gel/comet assay: guidelines for in vitro and in vivo genetic toxicology testing. Environ Mol Mutagen. 35: 206-221. 2000.
- Burlinson B, Tice RR, Speit G, Agurell E, Brendler-Schwaab SY, Collins AR, Escobar P, Honma M, Kumaravel TS, Nakajima M, Sasaki YF, Thybaud V, Uno Y, Vasquez M, Hartmann A, and In Vivo Comet Assay Workgroup potFIWoGT. Fourth International Workgroup on Genotoxicity testing: results of the in vivo Comet assay workgroup. Mutat Res. 627: 31-35. 2007.
- Lorenzo Y, Costa S, Collins AR, and Azqueta A. The comet assay, DNA damage, DNA repair and cytotoxicity: hedgehogs are not always dead. Mutagenesis. 28: 427-432. 2013.
- Morton D, Sellers RS, Barale-Thomas E, Bolon B, George C, Hardisty JF, Irizarry A, McKay JS, Odin M, and Teranishi M. Recommendations for pathology peer review. Toxicol Pathol. 38: 1118-1127. 2010.
- Mann P, and Hardisty JF. Peer Review and Pathology Working Groups. In: Haschek and Rousseaux’s Handbook of Toxicologic Pathology, W Haschek, C Rousseaux and M Wallig (eds). Academic Press, Amsterdam. 551-564. 2013.
- Burdock G. Fenaroli’s Handbook of Flavor Ingredients. 6th. ed. CRC Press, Boca Raton. 2010.
- Hobbs CA, Taylor SV, Beevers C, Lloyd M, Bowen R, Lillford L, Maronpot R, and Hayashi SM. Genotoxicity assessment of the flavouring agent, perillaldehyde. Food Chem Toxicol. 97: 232-242. 2016.
- Oser B, and Ford R. Recent progress in the consideration of flavoring ingredients under the Food Additives Amendment.11. GRAS substances. Food Technol. 32: 60-70. 1978.
- JECFA. Safety evaluation of certain food additives. In: Fifty-ninth Meeting of the Joint FAO/WHO Expert Committee on Food Additives. WHO Food Additive Series, no. 50., 2003.
- Cohen SM, Fukushima S, Gooderham NJ, Guengerich FP, Hecht SS, Rietjens I, Smith RL, Bastaki M, Harman CL, McGowen MM, and Taylor SV. FEMA expert panel review of p-mentha-1,8-dien-7-al genotoxicity testing results. Food Chem Toxicol. 98: 201-209. 2016.
- EFSA. EFSA Panel on food contact materials, enzymes, flavourings and processing aids scientific opinion on flavouring group evaluation 208 (FGE.208): consideration of genotoxicity data on representatives for 10 alicyclic aldehydes with the a,b-unsaturation in ring/side-chain and precursors from chemical subgroup 2.2 of FGE.19. EFSA J. 11: 3151. 2013.
- EFSA. EFSA Panel on food contact materials, enzymes, flavourings and processing aids scientific opinion on flavouring group evaluation 208 (FGE.208Rev1): consideration of genotoxicity data on representatives for 10 alicyclic aldehydes with the a,b-unsaturation in ring/side-chain and precursors from chemical subgroup 2.2 of FGE.19. EFSA J. 13: 4173. 2015.
- OECD. OECD Guideline for the Testing of Chemicals. TG474 Mammalian Erythrocyte Micronucleus Test. 2014.
- Beevers C. Final Report: p-Mentha-1,8-dien-7-al: Combined bone marrow micronucleus test and Comet assay in the liver of treated rats, Vol. Covance Laboratories, Ltd., North Yorkshire, UK. 2014.
- EFSA. Scientific Opinion on Flavouring Group Evaluation 226 Revision 1 (FGE.226Rev1): consideration of genotoxicity data on one a,b-unsaturated aldehyde from chemical subgrou 1.1.1(b) of FGE.19. EFSA Journal. 15: 4847 (4841-4824). 2017.
- JECFA. Safety evaluation of certain food additives. Sixty-fifth meeting of the Joint FAO/WHO Expert Committee on Food Additives. WHO Food Additives Series 56. 1-441. 2006.
- JECFA. Evaluation of certain food additives. Sixtyninth report of the Joint FAO/WHO Expert Committee on Food Additives. WHO Technical Report Series, no.952. 1-174. 2009.
- Beevers C. Final Report: 4,5-epoxydec-2(trans)-enal rat alkaline comet assay. Covance Study No 8331879, Vol. Covance Laboratories Ltd. , North Yorkshire, UK. 2016.
- Konishi Y, Hayashi SM, and Fukushima S. Regulatory forum opinion piece*: supporting the need for international harmonization of safety assessments for food flavoring substances. Toxicol Pathol. 42: 949-953. 2014.
Table 1. Comet assay results for male rats administered perillaldehyde
| Dose (mg/kg/day) |
% Tail DNA (mean ± SEM) |
% Hedgehogs (Mean) |
| 0 | 0.54 ± 0.15 | 7.17 |
| 175 | 0.72 ± 0.11 | 8.54 |
| 350 | 0.86 ± 0.11 | 6.96 |
| 700 | 2.20 ± 0.60***# | 9.04 |
| EMS (150) | 33.96 ± 1.38*** | 22.48 |
SEM = standard error of the mean EMS = ethyl methanesulfonate
*** p < 0.001 # p < 0.001 dose response test
Table 2. Comet assay results for male rats administered
4,5-epoxydec-2(trans)-enal
| Dose (mg/kg/day) |
% Tail DNA (mean ± SEM) |
% Hedgehogs (Mean) |
| 0 | 0.24 ± 0.07 | 1.17 |
| 75 | 0.85 ± 0.25* | 3.48 |
| 150 | 0.46 ± 0.23 | 1.93 |
| 300 | 1.06 ± 0.24**# | 2.68 |
| EMS (150) | 16.28 ± 1.24*** | 2.96 |
SEM = standard error of the mean EMS = ethyl methanesulfonate
* p < 0.05 ** p < 0.01 *** p < 0.001 # p < 0.05 dose response test
Figure 1. Irregular clear spaces in hepatocyte cytoplasm are consistent with intracytoplasmic glycogen storage in this liver from a vehicle control rat.
Figure 2. Hepatocytes are enlarged with small inform vacuoles consistent with microvesicular fat filling and expanding the cytoplasm and surrounding centrally located nuclei. Liver from a rat sacrificed 3 hours after 3rd daily gavage dose of 700 mg/kg of perillaldehyde.
Figure 3. Hypereosinophilic hepatocytes with condensed to pyknotic nuclei and shrunken angularly shaped cytoplasm (arrows) are randomly distributed among pale staining hepatocytes that are enlarged with cytoplasmic microvesicular fat vacuoles. The shrunken hypereosinophilic hepatocytes reflect different stages of hepatocellular death. Liver is from a rat sacrificed 3 hours after 3rd daily gavage dose of 700 mg/kg of perillaldehyde.
Figure 4. Normal liver with irregular clear areas in cytoplasm consistent with glycogen storage. Liver is from a vehicle control rat.
Figure 5. A normal area of liver showing absence of cytoplasmic glycogen from a rat sacrificed 3 hours after a second daily dose of 300 mg/kg of 4,5-epoxydec-2(trans)-enal.
Figure 6. Multiple hypereosinophilic hepatocytes with condensed cytoplasm, angular shapes, and condensed to pyknotic nuclei (arrows) from a rat sacrificed 3 hours after a second daily dose of 300 mg/kg of 4,5-epoxydec-2(trans)-enal. The shrunken hypereosinophilic hepatocytes reflect different stages of hepatocellular death.
Figure 7. Higher magnification of Figure 6 showing details of shrunken dying hepatocytes (arrows) from a rat sacrificed 3 hours after a second daily dose of 300 mg/kg of 4,5-epoxydec-2(trans)-enal.
Figure 8. A focal area of centrilobular hepatocellular necrosis with loss of normal hepatocellular structure and cells (asterisk). Liver from a rat sacrificed 3 hours after a second daily dose of 300 mg/kg of 4,5-epoxydec-2(trans)-enal.