An era can be defined as a period in time identified by distinctive character, events, or practices. We are now in the genomic era. The pre-genomic era: There was a pre-genomic era. It started many years ago with novel and seminal animal experiments, primarily directed at studying cancer. It is marked by the development of the two-year rodent cancer bioassay and the ultimate realization that alternative approaches and short-term animal models were needed to replace this resource-intensive and time-consuming method for predicting human health risk. Many alternatives approaches and short-term animal models were proposed and tried but, to date, none have completely replaced our dependence upon the two-year rodent bioassay. However, the alternative approaches and models themselves have made tangible contributions to basic research, clinical medicine and to our understanding of cancer and they remain useful tools to address hypothesis-driven research questions. The pre-genomic era was a time when toxicologic pathologists played a major role in drug development, evaluating the cancer bioassay and the associated dose-setting toxicity studies, and exploring the utility of proposed alternative animal models. It was a time when there was shortage of qualified toxicologic pathologists.The genomic era: We are in the genomic era. It is a time when the genetic underpinnings of normal biological and pathologic processes are being discovered and documented. It is a time for sequencing entire genomes and deliberately silencing relevant segments of the mouse genome to see what each segment controls and if that silencing leads to increased susceptibility to disease. What remains to be charted in this genomic era is the complex interaction of genes, gene segments, post-translational modifications of encoded proteins, and environmental factors that affect genomic expression. In this current genomic era, the toxicologic pathologist has had to make room for a growing population of molecular biologists. In this present era newly emerging DVM and MD scientists enter the work arena with a PhD in pathology often based on some aspect of molecular biology or molecular pathology research. In molecular biology, the almost daily technological advances require one’s complete dedication to remain at the cutting edge of the science. Similarly, the practice of toxicologic pathology, like other morphological disciplines, is based largely on experience and requires dedicated daily examination of pathology material to maintain a well-trained eye capable of distilling specific information from stained tissue slides – a dedicated effort that cannot be well done as an intermezzo between other tasks. It is a rare individual that has true expertise in both molecular biology and pathology. In this genomic era, the newly emerging DVM-PhD or MD-PhD pathologist enters a marketplace without many job opportunities in contrast to the pre-genomic era. Many face an identity crisis needing to decide to become a competent pathologist or, alternatively, to become a competent molecular biologist. At the same time, more PhD molecular biologists without training in pathology are members of the research teams working in drug development and toxicology. How best can the toxicologic pathologist interact in the contemporary team approach in drug development, toxicology research and safety testing? Based on their biomedical training, toxicologic pathologists are in an ideal position to link data from the emerging technologies with their knowledge of pathobiology and toxicology. To enable this linkage and obtain the synergy it provides, the bench-level, slide-reading expert pathologist will need to have some basic understanding and appreciation of molecular biology methods and tools. On the other hand, it is not likely that the typical molecular biologist could competently evaluate and diagnose stained tissue slides from a toxicology study or a cancer bioassay.The post-genomic era: The post-genomic era will likely arrive approximately around 2050 at which time entire genomes from multiple species will exist in massive databases, data from thousands of robotic high throughput chemical screenings will exist in other databases, genetic toxicity and chemical structure-activity-relationships will reside in yet other databases. All databases will be linked and relevant information will be extracted and analyzed by appropriate algorithms following input of the latest molecular, submolecular, genetic, experimental, pathology and clinical data. Knowledge gained will permit the genetic components of many diseases to be amenable to therapeutic prevention and/or intervention. Much like computerized algorithms are currently used to forecast weather or to predict political elections, computerized sophisticated algorithms based largely on scientific data mining will categorize new drugs and chemicals relative to their health benefits versus their health risks for defined human populations and subpopulations. However, this form of a virtual toxicity study or cancer bioassay will only identify probabilities of adverse consequences from interaction of particular environmental and/or chemical/drug exposure(s) with specific genomic variables. Proof in many situations will require confirmation in intact in vivo mammalian animal models. The toxicologic pathologist in the post-genomic era will be the best suited scientist to confirm the data mining and its probability predictions for safety or adverse consequences with the actual tissue morphological features in test species that define specific test agent pathobiology and human health risk.
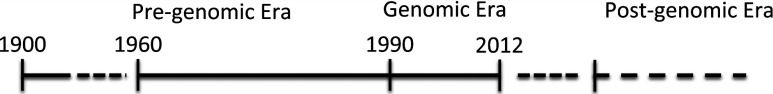
Fig. 1. Timeline representing the spans of the pre-genomic and genomic eras with a projection for the post-genomic era.
The Pre-Genomic Era
For practical purposes I have arbitrarily categorized the pre-genomic era as beginning around the year 1900 and ending in 1990. Prior to 1900, several key historical events identified environmental & occupational factors associated with cancer development in humans. In 1713 Bernadino Ramazzini, the father of occupational medicine, identified a high prevalence of breast cancer in nuns relate to nulliparity1. Perceival Pott documented occupational association of scrotal cancer in chimney sweeps in England in 17752. Further evidence linking a causative role of environmental exposure and cancer was reported by William Jackson Elmslie in 1866 when he linked induction of abdominal epitheliomas in Kashmir natives who sustained recurrent burns by warming themselves using braziers containing live coals held against their abdomen under their clothing3. Identification of the association of bladder cancer in aniline dye workers by Rehn in 1895 made us aware of the concept of chemical carcinogenesis associated with an industrial process4. Additional documentation of environmental or workplace exposures linked to cancer development followed over the next several years. Copies of the original papers for these and other seminal papers on experimental oncology are readily available2.
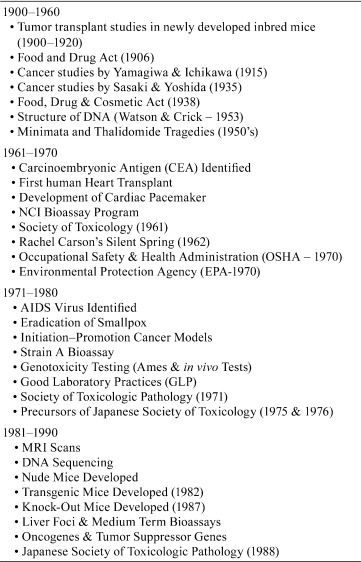
The pre-genomic era (~1900 to 1990) is characterized by several significant events and seminal animal experiments that constitute the historical underpinnings of toxicologic pathology. From the very beginning, many of these events focused on studies of cancer. The development of inbred mice and studies on transmission of spontaneously occurring cancer began in the U.S. at Harvard University and the Bussey Institute in the first two decades of the 1900’s and led to the establishment of the Jackson Laboratory in 1929 through the efforts of Clarence Cook Little5,6,7. The seminal publication by Yamagiwa and Ichikawa in 1915 in which they demonstrated that tar and soot (hydrocarbons & aromatic hydrocarbons) produced cancer on the skin of rabbits and mice, providing the first experimental evidence to confirm the observation by Perceival Pott in 17751,8. In 1925 Murphy and Sturm demonstrated skin-painting mice with polycyclic aromatic hydrocarbons led to systemic exposure with subsequent induction of lung tumors9. In 1935 Sasaki and Yoshida’s studies show that dietary administration of o-amidoazotoluene produced liver cancer in rats10. They further demonstrated the effects of dose on latency and carried out what is perhaps the earliest use of stop-exposure studies. Isaac Berenblum’s work in the early 1941’s defined the concept of co-carcinogenesis and early versions of the operational components of cancer, viz., initiation, promotion, and progression11. A variety of other biomedical and toxicological events characterized the pre-genomic era (Table 1).
One of the most notable events of direct relevance to toxicologic pathologists was the development of the two-year rodent cancer bioassay in the United States. The forerunner of the rodent cancer bioassay was established in 1961 at the National Cancer Institute (NCI) as a research-oriented program for investigating chemical carcinogenesis in animals with emphasis on chemical structures and structural classes12. The research priority was to gain insight into the etiology and mechanisms of chemical carcinogenesis. The following year a study of 120 pesticides and industrial intermediates was undertaken using two hybrid mouse strains. This study resulted in selection of the B6C3F1 mouse for subsequent NCI studies13. While these early studies lacked consistency and used small numbers of animals, by 1967 the rodent bioassay was standardized to include 50 rats and 50 mice per dose per sex. Initial studies were designed with a maximum tolerated dose (MTD) and one-half the MTD. Later studies included more doses, and in some studies included doses relevant to anticipated human exposure levels. Specific study modifications, including stop exposure groups and exposures beginning during gestation, were also introduced during this pre-genomic era. With the passage of the National Cancer Act in 1971 (referred to as President Nixon’s War on Cancer), funding was provided to start 60 full-scale rodent cancer bioassays followed by starting an unprecedented 200 more rodent bioassays in 1972. Needless to say, two-years later when these studies ended there was a tremendous backlog facing an insufficient number of toxicologic pathologists to carry out the pathology evaluations. The backlog was finally eliminated 4 years later12. The NCI rodent bioassay program was transferred to the National Toxicology Program in 1979.
Early during conduct of the two-year cancer bioassay it was realized that alternative approaches and short-term animal models might be identified as replacements for this resource-intensive and time-consuming method for identifying safety and predicting human health risk. Many past and contemporary alternative in vitro and in vivo approaches, short-term animal models, and coordinated efforts and strategies have been proposed to reduce reliance on the two-year rodent cancer bioassay (Table 2). To date, none of the proposed alternatives has replaced our dependence upon the two-year rodent bioassay. However, it is duly noted that the alternatives themselves have made tangible contributions to basic research and our understanding of cancer and remain useful tools to address hypothesis-driven research questions. The proposed alternative of an in vitro and in vivo genotoxicity battery approach has actually become a regulatory requirement for bringing new drugs and chemical entities to market. The pre-genomic era was also a time when the toxicologic pathologist played a major role in evaluating the cancer bioassay and its associated dose-setting toxicity studies as well as exploring the utility of the proposed in vivo animal model alternatives.
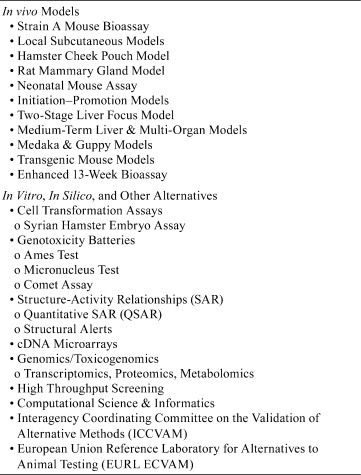
Table 2.
Past and Present Proposed Alternative Strategies to Reduce Reliance on the Two-Year Rodent Bioassay
The role of the toxicologic pathology throughout this pre-genomic era was to apply his or her expertise in the morphological characterization of the treatment-related tissue changes, including cancer. This has traditionally involved diagnosis of hematoxylin and eosin-stained tissue sections and integration with in-life and clinical data for overall interpretation at the conclusion of a toxicity or carcinogenicity animal study. Traditional medical and veterinary pathology training programs did not, and most still do not, provide specific training in the type of toxicologic pathology needed to evaluate the various animal toxicity and cancer testing studies. Thus, most of the toxicologic pathology training has occurred “on-the-job.”
Thus, the pre-genomic era can be summarized as a time period when epidemiological links between chemical exposures and human disease and life styles and human disease were identified and scientists began using animal studies to understand disease and predict potential risk for human disease. It was an era when the rodent cancer bioassay was used to identify safety of products already present or soon to be entering commerce. It was also the time when we began to search for alternatives to the resource-intensive 2-year rodent cancer bioassay and then realized that the various initially promising alternatives did not adequately fulfill enough of our hopes for a cost-effective, rapid, and relevant screening procedure to replace two-year rodent cancer studies. We also realized that the various animal studies were sometimes of questionable relevance to human health risk.
The Genomic Era
We are in the genomic era. The dividing line between the pre-genomic and the current genomic eras is not sharp, with carryover from the pre-genomic era. The genomic era started in the early 1990s and its science is progressing at warp speed. It is a time when the genetic underpinnings of normal biological and pathologic processes are being discovered and documented. We have moved beyond oncogenes and tumor suppressor genes to sequencing entire genomes and deliberately silencing relevant segments of that genome to see what each segment controls and if that silencing leads to increased susceptibility to disease. What remains to be charted in this genomic era is the complex interaction of genes, gene segments, post-translational modifications of encoded proteins, and effects of exposure on the epigenome.
Several significant biomedical and toxicological events occurred in the genomic era. In the biomedical arena we have seen the cloning of the sheep, Dolly; establishment of the human genome project and sequencing of the human genome; sequence of the mouse genome; and active research using stem cells. In the toxicological arena use of transgenic mouse bioassays; establishment of the International Conference on Harmonization (ICH); the “omics” revolution accompanied by anticipated excitement that toxicogenomics will lessen our dependence on conventional animal toxicity and carcinogenicity bioassays; high throughput screening of chemicals; and the building of informative databases to ultimately permit knowledge-based predictive toxicology14.
All this effort has created a new breed of researcher, the molecular biologist. The molecular biologist is a new player on the scene bringing the promise that teasing out the molecular underpinnings of toxicity and cancer induction by using molecular screening will quickly identify toxicities and obviate the necessity for as many animal studies. Many of the new scientists come from academic programs focused on molecular biology, without comprehensive veterinary or medical training, and with a type of “tunnel vision” centered on a particular molecular pathway. However, we are also generating DVM, PhD’s and MD, PhD’s with graduate credentials in molecular biology.
The newly emerging DVM and MD scientists enter the work arena with a PhD in pathology often based on a very focused aspect of molecular biology or molecular pathology research. For these individuals wishing to remain in the molecular research arena (in contrast to traditional diagnostic toxicologic pathologists), the almost daily advances in technology require complete dedication to remain at the cutting edge of molecular science. On the other hand, we have the diagnostic toxicologic pathologist.
Traditional diagnostic toxicologic pathology is a morphological discipline. Like other morphological disciplines, it is based largely on experience and requires fully engaged daily examination of pathology material to maintain a well-trained eye capable of distilling specific information from stained tissue slides, a dedicated effort that cannot be easily done as an intermezzo sandwiched between other tasks. It will be a rare individual that has in-depth expertise in molecular biology as well as finely honed skills in diagnostic pathology. In this genomic era, the newly emerging DVM-PhD or MD-PhD pathologist enters a marketplace without many job opportunities in contrast to the pre-genomic era. Many face a type of identity crisis needing to decide to become a competent diagnostic toxicologic pathologist or, alternatively, a competent molecular pathologist. It is hard for most to be excellent and at the cutting edge of both disciplines. At the same time, more PhD molecular biologists without training in pathology are members of the research teams working in drug development and toxicology. These individuals do not have the appropriate training and credentials to evaluate and render histopathological diagnoses. This necessitates that a sufficient population of certified toxicologic pathologists will be needed for diagnostic histopathology in support of toxicity and carcinogenicity studies and the anticipated development of specialized animal models.
How best can the toxicologic pathologist interact in the contemporary team approach in toxicology research and testing? Based on their biomedical training, toxicologic pathologists are in an ideal position to link data from the emerging technologies to their knowledge of pathobiology and toxicology. To effectively do this, the bench-level diagnostic pathologist, who is normally focused on slide-reading, will need to gain some basic understanding and appreciation of the contributions coming from the molecular biology component of the research team in order to appropriately integrate the molecular data with the in-life, postmortem, and diagnostic histopathology findings. The trick is for the diagnostic toxicologic pathologist to understand enough of the basics of molecular science to integrate molecular findings with in-life and postmortem findings. And for the molecular biologist, particularly those without veterinary or medical training, the trick is to know enough about organ-specific pathology to put the molecular findings into appropriate context. The solution is cross-disciplinary training for both of these members of the toxicology research team.
Cross-disciplinary training for members of the toxicology research team will be needed to efficiently and effectively develop new drug and chemical products and to ensure the safety of these products as well as the human health consequences from ubiquitous environmental exposures (e.g., air pollution, pesticide residues) and life style activities (e.g., radiofrequency exposure from use of cell phones). While cancer remains a critical focus of research, reproductive and developmental toxicology are now receiving more attention. Multiple disciplinary science provides the basis for contemporary teamwork to address complex disease and toxicity responses. Toxicologic pathology has and will continue to be a critical component in this multidisciplinary teamwork. Assuming that a typical toxicologic pathologist is not going to have the highest level of expertise on every topic relevant to drug development and safety assessment, an appropriate degree of cross-disciplinary exposure and training is and will continue to be necessary for one to remain a relevant member of the research team. The seasoned slide-reading toxicologic pathologist may be challenged by molecular biology’s fast changing lexicon and be uncomfortable with cluster analysis, heat maps, dendograms, oncogene point mutations or the latest type of RNA –– technologies that threaten to replace their experience-based judgment process. The younger toxicologic pathologist may have just completed a PhD degree, will probably have a good understanding of contemporary molecular technologies, but will not have received enough formal training in conventional toxicologic pathology or have logged enough time evaluating and peer reviewing conventional safety assessment study lesions. To be an effective part of a research team, the role for both the newly emerging and the veteran seasoned toxicologic pathologist is the same. Both need cross-disciplinary training. Escape is futile.
The source and answer to cross-disciplinary training is a concerted effort on the part of professional organizations and academic training programs to implement and encourage cross-cultural continuing education (CE). This is actually being done through formal CE courses for newly emerging omics-technologies and slide seminars for diagnostic training. However, more effort is needed, including support from company management to encourage their toxicologic pathologists to gain the additional training. The use of webinars and interactive tutorial sessions that are now possible in this electronic age along with use of whole slide digital images is encouraged. Participation of toxicologic pathologists in preparation of diagnostic atlases, such as the INHAND documents, is a means to provide diagnostic expertise in toxicologic pathology. Similar well designed training modules in molecular biology for pathologists are needed.
The use of conventional animal toxicity studies for predicting and assessing human health consequences has been a consistent concern from very early use of the rodent bioassay in the pre-genomic era and will remain a critical concern throughout the present genomic era. While there has always been concern about the high cost and lengthy features of the rodent bioassay, the more compelling concern is whether the rodent bioassay is of relevance for identifying human health risk. The toxicology community has shifted focus to the various omic technologies and robotic high throughput screening (HTS) of chemicals with the expectation that this new approach will reduce our reliance on animal bioassays. This has resulted in a paradigm shift in how we do toxicology and pathology research.
The potentially powerful omics-enabled technology, capable of producing enormous amounts of data and data sets, represents a significant shift in research methodology. Traditional research is driven by an initial hypothesis followed by a series of experiments to prove or disprove the hypothesis. The omics-approach, on the other hand, is capable of producing large data sets with the prospect that informative biomarkers and mechanistic insights gained from the massive amounts of data will allow generation of novel hypotheses for further investigation. This approach of looking for differences between control and test samples is an expedition in discovery, somewhat of an untargeted approach that ultimately will require extraction of hypotheses and the subsequent task of grinding out targeted data to address each hypothesis. To some degree it is easy to become enamored with omics-technology, getting caught up in expectations of great discoveries and definitive answers, thereby losing sight of toxicological question underlying the quest in the first place. Regardless of the motives behind this contemporary effort, the necessity to validate any insights revealed once the enormous data sets are analyzed will likely necessitate conventional toxicity studies requiring evaluation by toxicologic pathologists. This will be necessary in order to correlate potential molecular signatures with in vivopathology findings and relate any temporal molecular findings to long-term adverse outcomes. It is unlikely that gene arrays, related omics technologies, or high throughput screening will provided a sufficiently specific signature to obviate the need for histopathology in the foreseeable future.
Simultaneously with the development of the omics revolution and high throughput screening, the genetics community has been busy developing refined mouse models to more accurately reflect human genomic diversity. International efforts such as collaborative cross mice15, development of diversity outbred mice16, the international knockout mouse consortium (http://www.knockoutmouse.org), and an ever-increased introduction of humanized mice will generate thousands of new specialized animal models. These refined animal models are believed to be more relevant in predicting health consequences for exposed human populations. Just how the use of these refined mouse models will interface with contemporary toxicogenomic efforts remains to be seen in the coming years. What is going to be needed, however, is enough skilled toxicologic pathology diagnostic expertise to conduct the morphological and functional phenotyping of the newly emerging specialized rodent models and evaluate their performance in drug testing and in toxicity and carcinogenicity studies.
On another forefront of contemporary investigation is the prospect that toxicity studies utilizing human embryonic stem cells or induced pluripotent stem cells will allow assessment of effects of exposures on patterns of normal development. The potential of studies using stem cells will address developmental and other specialized toxicities (e.g. reproductive toxicity, neurotoxicity) and will require validation and use of specialized animal models requiring the diagnostic skills of toxicologic pathologists.
The Post-Genomic Era (An Elusive Future)
The post-genomic era will likely arrive at approximately 2050 at which time entire genomes from multiple species will exist in massive databases, data from thousands of robotic high throughput chemical screenings will exist in other databases, genetic toxicity and SAR will reside in yet other databases. All databases will be linked, relevant information will be extracted and analyzed by appropriate algorithms against the latest molecular, submolecular, genetic, experimental, and clinical data, and knowledge gained will permit the genetic components of many diseases to be amenable to therapeutic prevention and/or intervention. Much like computerized algorithms are currently used to forecast weather, to predict political elections, or to analyze the purchasing habits of individuals based on their electronic purchases and social interactions, computer driven sophisticated algorithms based largely on data mining will categorize new drugs and chemicals relative to their health and societal benefits versus health risks for defined human subpopulations. A new breed of scientist, the bioinformaticist, will emerge to effectively cross-link the various databases and extract predictive outcomes. However, just as computerized algorithms can only define probabilities of tomorrow’s or next week’s weather, accurately predicting adverse consequences from particular environmental and/or chemical/drug exposure(s) will require confirmation using intact in-vivo mammalian animal models. The toxicologic pathologist in the post-genomic era will be a pivotal link to integrate the in silico data mining and its probability predictions for safety or adverse consequences with actual tissue morphological features in test species to identify actual test agent pathobiology and human health risk.
Because of the diversity of the human population and the polygenic complexity of disease and toxicity response to exposure, multidisciplinary teamwork will remain essential in solving biomedical problems. The toxicologic pathologist will continue to be an essential part of multidisciplinary teams and is most suited to provide a leadership role in the post-genomic era. Assuming the current rate of progress, in another four or so decades we should be squarely in a post-genomic era. We, therefore, have time to prepare the discipline of toxicologic pathology for a leadership role in the post-genomic era. The veterinary and medical background training of toxicologic pathologists reflects a mindset that fosters evaluation and interpretation of complex data within the context of the whole organism biology. The background training in anatomy, physiology, and understanding of disease pathogenesis provides a basic understanding of cell, tissue, and whole organism response. What is currently lacking in veterinary and medical educational programs is specific subspecialty training in toxicologic pathology. Formal educational training in toxicologic pathology coupled with the toxicologic pathologist’s descriptive skills and knowledge of expected toxicities will allow for integration of predictive systems toxicology across species lines to identify features relevant to human disease. Toxicity studies, most likely in highly refined and humanized animal models, will require expert diagnostic pathology skills and ability for multidisciplinary integration of animal study data with input from database mining, computational science, and in silico predictive toxicology to identify relevant risk assessment for general as well as unique human subpopulations. The toxicologic pathologist with cross-disciplinary exposure to genetics, computational biology, and the next technology advances is ideally suited for leadership and integrator roles in the post-genomic era.
The practice and art of pathology based on diagnoses of hematoxylin and eosin-stained tissues hasn’t changed much since the early years of the pre-genomic era. In contrast, the genomic era has seen a rapid evolution of new genetic and molecular technologies, necessitating the need to reassess and redefine the role for pathologists in an ever-changing multidisciplinary milieu17,18,19. As toxicologic pathologists our challenge is to seize the opportunity to take advantage of our unique background and experience and assume a leadership role in synergizing the multidisciplinary team contributions such that the whole is greater than the sum of the parts.
Footnotes
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (by-nc-nd) License <http://creativecommons.org/licenses/by-nc-nd/3.0/>.
References
1. Shimkin M. Contrary to Nature. DHEW Publication No. (NIH) 76-720, National Institutes of Health, Bethesda. 91. 1977
2. Shimkin M. Some Cassics of Experimental Oncology: 50 selections. DHEW Pub (NIH) 80-2150, National Institutes of Health, Bethesda. 739. 1980
3. Elmslie W. Etiology of epithelioma among the Kashmiris. Indian Med Gaz. 1: 324–326 1866
4. Rehn L. Bladder tumors in fuchsin workers (from German). Archiv für Klinische Chirurgie. 50: 588–600 1895
5. Barthold SW. Microbes and the evolution of scientific fancy mice. ILAR J. 49: 265–271 2008.
6. Rao G., and Boorman G. History of the B6C3F1 mouse. In: Pathology of the Mouse. R Maronpot (ed). Cache River Press, Vienna. 1–6. 1999
7. Guenet JL., and Bonhomme F. Origin of the laboratory mouse and related subspecies. In: The Laboratory Mouse. H Hedrich, and G Bullock (eds). Elsevier, Amsterdam. 3–13. 2004
8. Yamagiwa K., and Ichikawa K. Experimental study of the pathogenesis of carcinoma. Cancer Res. 3: 1–29 1918
9. Murphy JB., and Strum E. Primary lung tumors in mice following the cutaneous application of coal tar. J Exp Med. 42: 693–700 1925.
10. Sasaki T., and Yoshida T. Liver carcinoma induced by feeding o-amidoazotuluene (from German). Virch Arch Patholog Anat. 295: 175–200 1935
11. Berenblum I. The mechanism of carcinogenesis: A study of the significance of cocarcinogenic action and related phenomena. Cancer Res. 1: 807–814 1941
12. Weisburger EK. History of the bioassay program of the national cancer institute. Prog Exp Tumor Res. 26: 187–201 1983.
13. Innes JR., Ulland BM., Valerio MG., Petrucelli L., Fishbein L., Hart ER., Pallotta AJ., Bates RR., Falk HL., Gart JJ., Klein M., Mitchell I., and Peters J. Bioassay of pesticides and industrial chemicals for tumorigenicity in mice: A preliminary note. J Natl Cancer Inst. 42: 1101–1114 1969.
14. Waters M., and Merrick B. Toxicogenomics and the evolution of systems toxicology. In: General and Applied Toxicology. B Ballantyne, T Marrs, and T Syversen (eds). John Wiley & Sons, Chichester. 2009
15.Threadgill DW, and Churchill GA. Ten years of the collaborative cross. G3. 2: 153-156. 2012.
16. Churchill GA., Gatti DM., Munger SC., and Svenson KL. The diversity outbred mouse population. Mamm Genome. 23: 713–718 2012.
17. Boorman GA., Anderson SP., Casey WM., Brown RH., Crosby LM., Gottschalk K., Easton M., Ni H., and Morgan KT. Toxicogenomics, drug discovery, and the pathologist. Toxicol Pathol. 30: 15–27 2002.
18. Ettlin RA., and Leininger JR. Toxicologic pathology in the new millennium. Toxicol Pathol. 30: 160–163 2002.
19. Morgan KT., Pino M., Crosby LM., Wang M., Elston TC., Jayyosi Z., Bonnefoi M., and Boorman G. Complementary roles for toxicologic pathology and mathematics in toxicogenomics, with special reference to data interpretation and oscillatory dynamics. Toxicol Pathol. 32(Suppl 1): 13–25 2004.