The following three articles represent the output of a combined effort initiated by the Scientific Regulatory Policy Committee of the Society of Toxicologic Pathology to provide a unified review of current scientific practices and relevant literature and provide suggestions regarding the recognition, interpretation, and risk assessment of hepatic drug metabolizing enzyme (DME) induction studies. The core objective was to provide a review that the scientific community including pathologists, regulatory scientists, toxicologists, investigative scientists, and others would find valuable for managing, designing, and interpreting toxicity studies supporting regulatory filings. Three working groups composed of scientists from industry, academia, and regulatory agencies were convened to review the available literature on important aspects of the interpretation and risk assessment of hepatic microsomal DME enzyme induction in three publications. The three reviews are as follows:
‘‘Effects of Hepatic Drug Metabolizing Enzyme Induction on Clinical Pathology Parameters in Animals and Man,’’ Toxicol Pathol
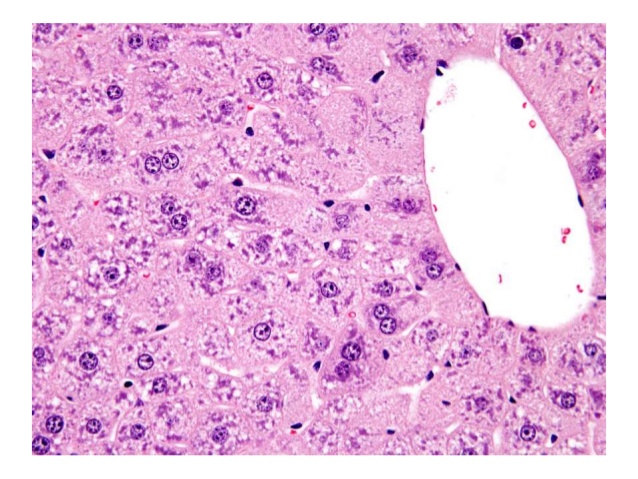
‘‘Hepatic Drug Metabolizing Enzyme Induction: Microscopic and Ultrastructural Appearance,’’ Toxicol Pathol
‘‘Hepatic Drug Metabolizing Enzyme Induction and Implications for Preclinical and Clinical Risk Assessment,’’ Toxicol Pathol
The purpose of this introduction is not to summarize the articles but rather to frame the series and to provide a common mechanistic introduction.
Keywords
hepatic drug metabolizing enzyme induction.
Enzyme induction affects mainly two types of enzyme systems in mammalian species: enzymes that are constitutively expressed for maintenance of basic life functions and enzymes that are synthesized or repressed in response to xenobiotic or endobiotic stimuli including environmental chemicals, drugs, or endogenous molecules. For purposes of the following three reviews, enzyme induction is defined as an increase in the activity of a drug metabolizing enzyme (DME).
The liver is the major site of xenobiotic metabolism in mammals. The liver is also one of the primary organs responsible for maintenance of normal homeostasis and physiological functions and, as a dynamic system, is capable of relatively rapid responses to stimuli including DME induction. Hepatic DME induction may be associated with changes in liver weight, histological evidence of hepatocellular hypertrophy or hyperplasia, and/or elevation of serum clinical chemistry analytes. Enzyme induction may or may not be associated with target organ toxicity.
The most common mechanism of DME induction is derepression of genes responsible for enzyme synthesis; however, other mechanisms can also be responsible for amplified levels of enzymes following exposure to inducer xenobiotics. Enzyme inducers can increase levels of metabolizing enzymes that act on the inducer itself (autoinduction) or on other substrates. Depending upon the specific xenobiotic, the effect of enzyme induction can range from a benign adaptive response to generation of highly reactive toxic metabolites. This effect can also depend on the sex and species being exposed, the dose and the frequency of exposure, diet and age of the animal, and other factors.
In drug development, induction of DMEs, particularly of the cytochrome P450 family, is a relatively common event that in preclinical safety testing can be associated with a number of adverse outcomes including hepatotoxicity and carcinogenesis (Handschin and Meyer 2003). Clinically, xenobiotic metabolizing enzyme induction has historically focused on the potential for drug–drug interaction or bioactivation specific to a xenobiotic because these are the most common undesired effects of DME. However, consequences associated with DME induction in humans have received increased attention for contributing to a wide range of effects including altered pharmacokinetics and, less commonly, toxicity (Fuhr 2000).
Biotransformation reactions increase the solubility of lipophilic substances and are subdivided into phase I and phase II reactions. Phase I reactions expose or add polar functional groups through hydrolysis, reduction, or oxidation reactions and are primarily performed by cytochrome P450 mixed-function oxidases (CYPs) of the endoplasmic reticulum or microsomal fraction. Phase II reactions primarily increase hydrophilicity of substrates and need not be preceded by phase I reactions for substrates with appropriate functional groups. Elimination of phase II metabolites occurs in phase III reactions by adenosine triphosphate (ATP)- dependent transporters in liver, intestine, and kidney (Handschin and Meyer 2003). The coordinated regulation of phase I and II enzymes and phase III transporters occurs by cross-talk between shared signalling molecules or patterns of transcriptional activation common to both sets of enzymes (Xu, Li, and Kong 2005).
The most significant induction of DMEs results from increased gene transcription via ligand-dependent activation of nuclear receptors or transcription factors (Honkakoski and Negishi 2000; Xu, Li, and Kong 2005). The dominant receptors in this process are the Aromatic hydrocarbon Receptor (AhR), Pregnane X-Receptor (PXR), Constitutive Androstane Receptor (CAR), and Peroxisome Proliferator Activated ReceptorAlpha (PPARα). Because CYPs are the best-characterized and most important DMEs in terms of number and types of substrates, the phenomenon of enzyme induction is commonly assessed by quantifying CYP mRNA, protein, or enzymatic activity (Dickins 2004). However AhR, CAR, PXR, and PPARα also regulate expression of phase II enzymes including uridine diphosphoglucuronsyltransferases, enzymes that are responsible for the majority of conjugation reactions with therapeutic drugs, as well as glutathione transferases and sulfotransferases (Handschin and Meyer 2003).
The regulation of expression of different CYPs is mediated by different transcription factors: the AhR predominantly regulates the CYP1A subfamily (Whitlock 1999), CAR mainly regulates the CYP2B family (Wang and Negishi 2003), PXR mainly regulates the CYP3A subfamily (Kliewer 2003) and PPARα regulates the CYP4A subfamily (Dickins 2004; Aldridge, Tugwood, and Green 1995). These associations are not absolute, and there is clear evidence of receptor cross-talk, especially between PXR and CAR (Pascussi et al. 2003).
The identification of the molecular mechanisms for induction of DMEs has led to a greater understanding of the wider biological consequences and species differences in this response. Both structural and functional differences in nuclear receptor activity exist across species and within species between sexes (Martignoni, Groothuis, and de Kanter 2006). These functional differences are largely related to differences in the ligand binding domain, as PXR and CAR exhibit the greatest structural diversity of all of the nuclear receptors across species, with approximately 76% and 72% sequence homology between rodent and human for PXR and CAR, respectively (Kretschmer and Baldwin 2005; Moore et al. 2003; Dickins 2004).
It is important to note that with the exception of CYP2E1, which has only one known isoform and shows no appreciable difference in catalytic activity across species (Guengerich 1997; Bogaards et al. 2000), none of the animal species are completely similar to man with respect to the CYP induction profile in response to xenobiotics. For members of the CYP1A family, all species express CYP1A1 and CYP1A2, albeit to a different extent and with different induction responses (Martignoni, Groothuis, and de Kanter 2006). Substantial differences exist across species in expression, catalytic activity, and organ distribution of CYP2C, CYP2D, and CYP3A isoforms. However, compared to man, dog is most similar in induction responses for CYP2D; monkey for CYP2C; rat and mouse for CYP1A; and rat, mouse, and pig for CYP3A (Bogaards et al. 2000; Martignoni, Groothuis, and de Kanter 2006; Zuber, Anzenbacherova, and Anzenbacher 2002).
The following three articles provide a comprehensive review of the clinico-pathologic and morphologic consequences of hepatic DME induction and its role in risk mitigation for human safety during drug development, assessment of environmental health, and safety.
References
Aldridge, T. C., Tugwood, J. D., and Green, S. (1995). Identification and characterization of DNA elements implicated in the regulation of CYP4A1 transcription. Biochem J 306 (Pt. 2), 473–79.
Bogaards, J. J., Bertrand, M., Jackson, P., Oudshoorn, M. J., Weaver, R. J., van Bladeren, P. J., and Walther, B. (2000). Determining the best animal model for human cytochrome P450 activities: A comparison of mouse, rat, rabbit, dog, micropig, monkey and man. Xenobiotica 30, 1131–52.
Dickins, M. (2004). Induction of cytochromes P450. Curr Top Med Chem 4, 1745–66.
Fuhr, U. (2000). Induction of drug metabolising enzymes: Pharmacokinetic and toxicological consequences in humans. Clin Pharmacokinet 38, 493–504.
Guengerich, F. P. (1997). Comparisons of catalytic selectivity of cytochrome P450 subfamily enzymes from different species. Chem Biol Interact 106, 161–82.
Handschin, C., and Meyer, U. A. (2003). Induction of drug metabolism: The role of nuclear receptors. Pharmacol Rev 55, 649–73.
Honkakoski, P., and Negishi, M. (2000). Regulation of cytochrome P450 (CYP) genes by nuclear receptors. Biochem J 347, 321–37.
Kliewer, S. A. (2003). The nuclear pregnane X receptor regulates xenobiotic detoxification. J Nutr 133, 2444S–7S.
Kretschmer, X. C., and Baldwin, W. S. (2005). CAR and PXR: Xenosensors of endocrine disrupters? Chem Biol Interact 155, 111–28.
Martignoni, M., Groothuis, G. M., and de Kanter, R. (2006). Species differences between mouse, rat, dog, monkey and human CYP-mediated drug metabolism, inhibition and induction. Expert Opin Drug Metab Toxicol 2, 875–94.
Moore, J. T., Moore, L. B., Maglich, J. M., and Kliewer, S. A. (2003). Functional and structural comparison of PXR and CAR. Biochim Biophys Acta 1619, 235–8.
Pascussi, J. M., Gerbal-Chaloin, S., Drocourt, L., Maurel, P., and Vilarem, M. J. (2003). The expression of CYP2B6, CYP2C9 and CYP3A4 genes: A tangle of networks of nuclear and steroid receptors. Biochim Biophys Acta 1619, 243–53.
Wang, H., and Negishi, M. (2003). Transcriptional regulation of cytochrome p450 2B genes by nuclear receptors. Curr Drug Met 4, 515–25.
Whitlock, J. P., Jr. (1999). Induction of cytochrome P4501A1. Ann Rev Pharmacol Toxicol 39, 103–25.
Xu, C., Li, C. Y., and Kong, A. N. (2005). Induction of phase I, II and III drug metabolism/transport by xenobiotics. Arch Pharm Res 28, 249–68.
Zuber, R., Anzenbacherova, E., and Anzenbacher, P. (2002). Cytochromes P450 and experimental models of drug metabolism. Cell Mol Med 6, 189–98.